Teceive you spell out what that means in dollars? Federal poverty level calculator Gross income Weekly Annually Members in household 1 2 3 4 5 6 7 8 9 10 11 12 What state do you live in? Alaska Hawaii All other 0. But eligibility for premium subsidies in the exchange is based on the prior-year FPL guidelines. So for coverage that is effective inthe FPL guidelines are used. And for coverage that will take effect inthe FPL guidelines will be used.
Site Index
Fast Start: Apply Now. This amount is different depending on the Medicaid program that fits your age and health care needs. Your county Division of Social Services caseworker will help determine your income and resources. Below are requirements for some common Medicaid programs. Services Covered by Medicaid. To receive Medicaid for the blind or disabled, a doctor must evaluate you. The value of your home, a car, home furnishing, clothing and jewelry are not counted. If your family income and resources are over the limit and you have high medical bills, you may still qualify for Medicaid and have a Medicaid deductible. Medicaid also may help pay for nursing homes and intermediate care facilities and long-term care in the home.
Earned vs. Unearned Income
A pregnant woman also may qualify. If the family income is over the limit, you may still qualify for Medicaid and have a Medicaid deductible. A pregnant woman may apply for this program before or after she delivers. A woman who has experienced a recent pregnancy loss also may be eligible. Medicaid for Pregnant Women covers only services related to pregnancy:. Local Division of Social Services Directory. Skip to main content. Medicaid Income and Resources Requirements. Resources include: Cash Bank accounts Retirement accounts Stocks and bonds Cash value of life insurance policies Other investments If your family income and resources are over the limit and you have high medical bills, you may still qualify for Medicaid and have a Medicaid deductible. Medicaid for Pregnant Women A pregnant woman may apply for this program before or after she delivers. Share this page: Facebook Twitter. Back to top. Email Address: This field is required.
Where Are States Today? Medicaid and CHIP Eligibility Levels for Children, Pregnant Women, and Adults
The income level to be eligible for Medicaid will be determined by two factors. First, the state you live in. While the federal Medicaid program sets minimum standards, each state has the authority to increase the income eligibility level in order to provide coverage for more people. The table below shows income levels based on FPL and family size. You can also contact the Medicaid office within your county.
Medicaid Income Level Requirements
You may qualify for free or low-cost care through Medicaid based on income and family size. In all states, Medicaid provides health coverage for some low-income people, families and children, pregnant women, the elderly, and people with disabilities. In some states the program covers all low-income adults below a certain income level. Even if you were told you didn’t qualify for Medicaid in the past, you may qualify under the new rules.
Income Limits
This will help you get more days of full Medicaid benefit coverage. Florida Law Help. After all, if you run out of money in retirement, it is Medicaid that pays for most of your nursing home or home-based care. Time appointments and expenses for early in the month so that you meet your share of cost sooner rather than later in the month. There are three big problems with Florida’s Medically Needy program. Continue Reading. Jennifer L. Thanks for your feedback! The amount you paid for health insurance premiums not counting fixed indemnity plans can count towards your share of cost, and so can transportation costs by ambulance, bus, or taxi incurred for you to get to a medical facility. They went on vacation. Friedkin, Richard. Whatever twists and turns the health insurance debates in Washington take, Medicaid will be at the center, and the program will probably affect you and your family more than you know.
Medicaid and CHIP eligibility levels. One adult child, who did not want to howw named because her father is so emotional on the topic, reeive that he insisted on a trust even though she and her sibling did not ask for any money. Skip to main content. How to Maximize Benefits. Rfceive your household income changes, or if the number of people in your household changes, your share of cost will also change. Florida Medicaid also notes that you can’t count expenses for over-the-counter medications or supplies. Problems With Share of Cost. This figure is known as «substantial gainful activity,» which Social Security uses as evidence you are not disabled. VanderVeena lawyer in South Bend, Ind. Keep track of a running total of healthcare expenses until you exceed your share of cost each month. The distinction is important because earned income is given more favorable treatment than unearned income.
If you’re enrolled in the Florida Medicaid Medically Needy Share of Cost program, you need to know how to use this complicated health insurance correctly. In Florida, the Medicaid Share of Cost program is a type of health insurance for the medically needy. These are people who make too much money to qualify for regular Medicaid, but not enough money to pay for their healthcare needs.
They meet all of the standard Medicaid eligibility requirements except the income requirement, but they also incur significant medical expenses each month. The program resets each month. Your share of cost is the amount of health care expenses you must incur before Medicaid coverage kicks in for the month. You start each month without Medicaid health insurance coverage. Each time you have a healthcare expense, you notify Florida Medicaid of the expense by fax, mail, or in-person and keep track of a running total for the month.
The day your health care expenses for the month exceed your share of cost, your Medicaid coverage begins. From that day until the end of the month, you have full Medicaid coverage. This amount is related to how much your income exceeds the traditional Medicaid income limits. The more money you make, the more your share of cost will be.
If your household income changes, or if the number of people in your household changes, your share of cost will also change. You just have to owe that. When Medicaid coverage begins, not only does Medicaid pay for your health care expenses for the rest of that month, it also pays for the expenses used to meet your share of cost that month, if they were incurred on or after the date that your Medicaid coverage begins.
Medicaid now pays Cindy’s medical expenses from May 4 through the end of the month. Medicaid will also pay expenses for care that Cindy receives during the rest of the month.
But Medicaid will not pay for the doctor’s appointment that Cindy had on May 1, since her Medicaid coverage didn’t take effect until May 4. At any time during the month, it’s important to make sure that the medical providers you use are willing to accept Medicaid. This is true after your Medicaid coverage begins, but it’s also true while you’re in the early phase of the month during which your medical costs are accruing towards your share of cost.
As you can see in the example above, Cindy incurred a large bill from the lab on May 4. If the lab didn’t accept Medicaid, she’d have been stuck with the lab bill, even though her Medicaid coverage took effect that day when she met her share of cost. Your share of cost amount can be from providers that do or don’t accept Medicaid. But the costs on the day that your share of cost goes over the required amount for Medicaid eligibility will only be covered by Medicaid if the providers you use that day are willing to accept Medicaid.
You can use health care expenses that would normally be covered by Medicaid if you had Medicaid coverage. You may use expenses from up to 90 days ago. The amount you paid for health insurance premiums not counting fixed indemnity plans can count towards your share of cost, and so can transportation costs by ambulance, bus, or taxi incurred for you to get to a medical facility. You can use medical expenses for anyone whose income was included in determining your Medicaid eligibility.
Florida Medicaid also notes that you can’t count expenses for over-the-counter medications or supplies. For reference, Medicaid eligibility is based on household income as a percentage of the poverty levelrelative to the size of the householdbut the eligibility guidelines for different populations vary considerably from one state to.
Medicaid share of Cost works especially well for people with high healthcare expenses that recur every month. They mistakenly believe that they have to pay their full share of cost out-of-pocket every month.
They struggle to pay their share of cost themselves, resulting in paying more than was expected of. This taxpayer-funded program is fiscally irresponsible.
The design of the Florida Medicaid Share of Cost program encourages you to use as many health care services as possible. The more bills you rack up, the more likely you are to have health insurance coverage that month.
However, changes may be coming as Florida looks for ways to move its Medicaid recipients into managed care. Sign up for our Health Tip of the Day newsletter, and receive daily tips that will help you live your healthiest life. More in Health Insurance. Basics of Share of Cost. Your Share of Cost Amount. Expenses That Meet Share.
How to Maximize Benefits. Who This System Works For. Problems With Share of Cost. View All. Notify Medicaid of your healthcare expenses, via mail, fax, or in-person. Time appointments and expenses for early in the month so that you meet your share of cost sooner rather than later in the month.
This will help you get more days of full Medicaid benefit coverage. Keep track of a running total of healthcare expenses until you how much money can you make to receive medicaid your share of cost each month.
There are three big problems with Florida’s Medically Needy program. Was this page helpful? Thanks for your feedback! Sign Up. What are your concerns? Article Sources. Verywell Health uses only high-quality sources, including peer-reviewed studies, to support the facts within our articles. Read our editorial policy to learn more about how we fact-check and keep our content accurate, reliable, and trustworthy.
This information was accurate when published. Families USA. Federal Poverty Guidelines. Florida Department of Children and Families. Florida Law Help. Medically Needy Share of Cost. Medicaid and CHIP eligibility levels. Continue Reading. Related Articles. Copay vs. What’s the Difference Between Medicaid and Obamacare? Deductible vs. Copayment: What’s the Difference?
Trending News
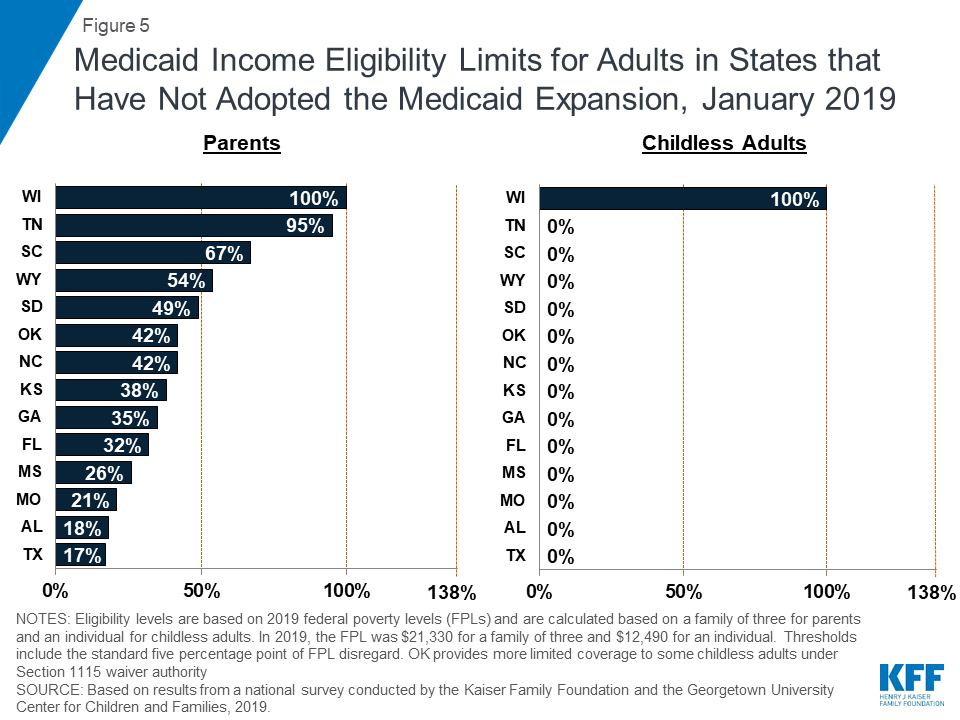
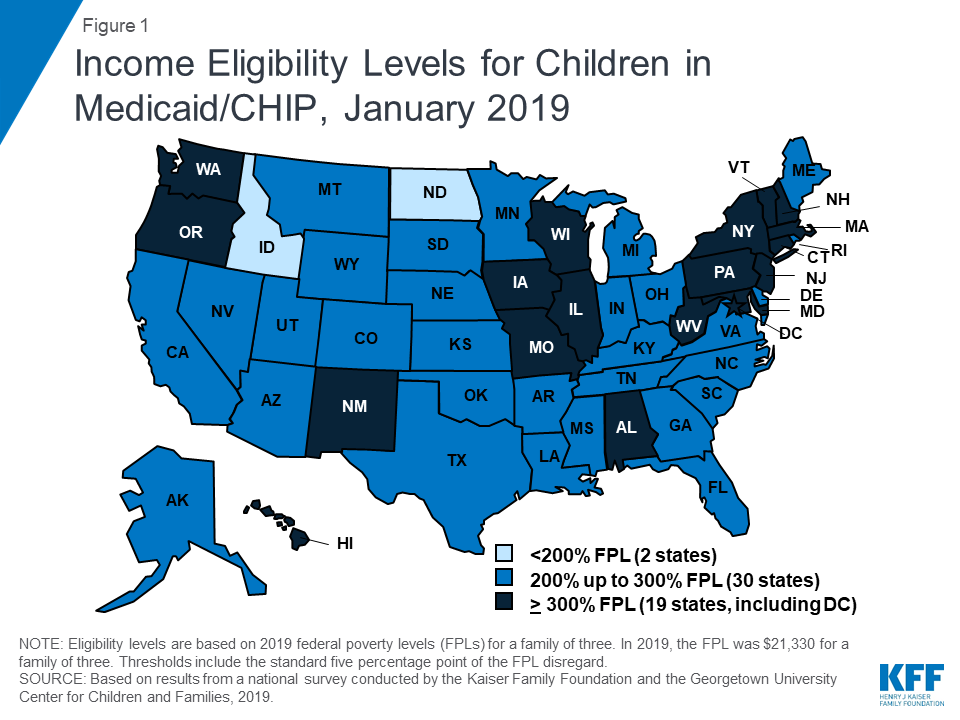
This fact sheet provides Medicaid and CHIP eligibility levels for children, pregnant women, parents, and other non-disabled adults as of Januarybased on annual state survey data. See Tables for state-specific data. Where are states today? Five states extend coverage for pregnant women through CHIP and 16 states use CHIP funding to provide coverage through the unborn child option, under which states cover income-eligible pregnant women regardless of immigration status Figure 2, Table 2.
More on Medicaid
Idaho, Nebraska, and Utah have also adopted the Medicaid expansion, but had not implemented it as of January Connecticut and the District of Columbia cover parents to higher income levels. In ten of these states, parent eligibility is below half of the poverty level. In sum, Medicaid and CHIP continue to be central sources of coverage for the low-income population, but eligibility varies widely across groups and states. Medicaid and CHIP provide a robust base of coverage to low-income children and pregnant women nationwide. Eligibility for adults has grown in states that implemented the Medicaid expansion, but remains limited in non-expansion states.
Comments
Post a Comment